Write text here...
Heart Disease Facts
Postado por Unknown | 04:34 | Cardiovascular Disorders, Conditions and Diseases, Coronary artery bypass surgery, Health, Heart disease, Hypertension, Myocardial infarction, United States | 0 comentários »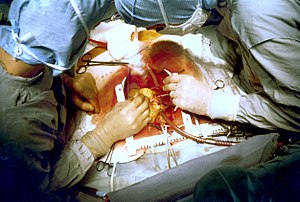 Image via Wikipedia
Image via Wikipedia
Heart Disease Facts
- Heart disease is the leading cause of death for both women and men in the United States.1
- In 2005, 652,091 people died of heart disease (50.5% of them women). This was 27.1% of all U.S. deaths. The age-adjusted death rate was 222 per 100,000 population.1
- Heart disease is the leading cause of death for American Indians and Alaska Natives, blacks, Hispanics, and whites. For Asians and Pacific Islanders, cancer is the leading cause of death (accounting for 27.5% of all deaths), heart disease is a close second (25.0%).2
- Heart disease crude death rates per 100,000 population for the five largest U.S. racial/ethnic groups are as follows: Hispanics, 69.2; Asians and Pacific Islanders, 73; American Indians, 82.5; blacks, 189.8; and whites, 235.5.2
- In 2005, the age-adjusted death rates for diseases of the heart was 211.1 deaths per 100,000 for all Americans. The age-adjusted death rate for whites was 207.8, and 271.3 for African Americans. Age adjusted rates are used to compare populations with differeing age distributions.2
- By state, age-adjusted death rates per 100,000 for diseases of the heart ranged from 141.1 (Minnesota) to 306.8 (Mississippi) in 2005.1
- Coronary heart disease is the principal type of heart disease. In 2005, 445,687 people that died from coronary heart disease. That is about 68.3% of all heart disease deaths.5
- It is estimated that about 47% of cardiac deaths occur before emergency services or transport to a hospital.4
- In 2009, heart disease is projected to cost more than $304.6 billion, including health care services, medications, and lost productivity.5
- Worldwide, coronary heart disease killed more than 7.6 million people in 2005.6
- Risk factors for heart disease among adults (for years 2003–2004 unless noted, age-adjusted):3
Percentage of persons aged 20 years and older with hypertension or taking hypertension medications: 32.1%
Percentage of persons aged 20 years and older with high blood cholesterol: 16.9%
Percentage of persons aged 20 years and older with physician-diagnosed diabetes: 10.0%
Percentage of persons aged 20 years and older who are obese: 32.0%
Percentage of adults aged 18 years and older who are current cigarette smokers (2004-2006): 18.4%
Percentage of adults aged 18 years and older who engage in no leisure-time physical activity (2006): 39.5%
- In 2003, approximately 37% of adults reported having two or more of six risk factors for heart disease and stroke (high blood pressure, high cholesterol, diabetes, current smoking, physical inactivity, and obesity).7
- Timely access to emergency cardiac care and survival is partly dependent on early recognition of heart attack symptoms and immediate action by calling emergency services. In a 2005 survey, most persons (92%) recognized chest pain as a heart attack symptom, but only 27% correctly classified all symptoms and knew to call 9–1–1 when someone was having a heart attack.8
- Studies among people with heart disease have shown that lowering high blood cholesterol and high blood pressure can reduce the risk of dying of heart disease, having a nonfatal heart attack, and needing heart bypass surgery or angioplasty.
- Studies among people without heart disease have shown that lowering high blood cholesterol and high blood pressure can reduce the risk of developing heart disease.
Symptoms of Heart Disease
Postado por Unknown | 04:32 | Atrial fibrillation, Cardiac arrhythmia, Cardiovascular Disorders, Conditions and Diseases, Health, Heart disease, Heart failure, Palpitation | 0 comentários » Image via Wikipedia
Image via Wikipedia
Coronary artery disease, heart attack -- each type of heart disease has different symptoms, although many heart problems have similar warning signs. The symptoms you experience depend on the type and severity of your heart condition. Learn to recognize your symptoms and the situations that cause them. Call your doctor if you begin to have new symptoms or if they become more frequent or severe.
Symptoms of Coronary Artery Disease
The most common symptom of coronary artery disease is angina, or chest pain. Angina can be described as a discomfort, heaviness, pressure, aching, burning, fullness, squeezing, or painful feeling in your chest. It can be mistaken for indigestion or heartburn. Angina is usually felt in the chest, but may also be felt in the shoulders, arms, neck, throat, jaw, or back.
Other symptoms of coronary artery disease include:
- Shortness of breath
- Palpitations (irregular heart beats, skipped beats, or a "flip-flop" feeling in your chest)
- A faster heartbeat
- Weakness or dizziness
- Nausea
- Sweating
Symptoms of a Heart Attack (Myocardial Infarction or MI)
Symptoms of a heart attack can include:
- Discomfort, pressure, heaviness, or pain in the chest, arm, or below the breastbone
- Discomfort radiating to the back, jaw, throat, or arm
- Fullness, indigestion, or choking feeling (may feel like heartburn)
- Sweating, nausea, vomiting, or dizziness
- Extreme weakness, anxiety, or shortness of breath
- Rapid or irregular heartbeats
During a heart attack, symptoms typically last 30 minutes or longer and are not relieved by rest or oral medications (medications taken by mouth). Initial symptoms can start as a mild discomfort that progresses to significant pain.
Some people have a heart attack without having any symptoms (a "silent" MI). A silent MI can occur among all people, though it occurs more often among diabetics.
If you think you are having a heart attack, DO NOT DELAY. Call for emergency help (dial 911 in most areas). Immediate treatment of a heart attack is very important to lessen the amount of damage to your heart.
Symptoms of Arrhythmias
When symptoms of arrhythmias, or an abnormal heart rhythm, are present, they may include:
- Palpitations (a feeling of skipped heart beats, fluttering or "flip-flops," or feeling that your heart is "running away").
- Pounding in your chest.
- Dizziness or feeling light-headed.
- Fainting.
- Shortness of breath.
- Chest discomfort.
- Weakness or fatigue (feeling very tired).
Symptoms of Atrial Fibrillation
Atrial fibrillation (AF) is a type of arrhythmia. Most people with AF experience one or more of the following symptoms:
- Heart palpitations (a sudden pounding, fluttering, or racing feeling in the heart).
- Lack of energy; tired.
- Dizziness (feeling faint or light-headed).
- Chest discomfort (pain, pressure, or discomfort in the chest).
- Shortness of breath (difficulty breathing during activities of daily living).
Some patients with atrial fibrillation have no symptoms. Sometimes these episodes are briefer.
Symptoms of Heart Valve Disease
Symptoms of heart valve disease can include:
- Shortness of breath and/or difficulty catching your breath. You may notice this most when you are active (doing your normal daily activities) or when you lie down flat in bed.
- Weakness or dizziness.
- Discomfort in your chest. You may feel a pressure or weight in your chest with activity or when going out in cold air.
- Palpitations (this may feel like a rapid heart rhythm, irregular heartbeat, skipped beats, or a flip-flop feeling in your chest).
If valve disease causes heart failure, symptoms may include:
- Swelling of your ankles or feet. Swelling may also occur in your abdomen, which may cause you to feel bloated.
- Quick weight gain (a weight gain of two or three pounds in one day is possible).
Symptoms of heart valve disease do not always relate to the seriousness of your condition. You may have no symptoms at all and have severe valve disease, requiring prompt treatment. Or, as with mitral valve prolapse, you may have severe symptoms, yet tests may show minor valve disease.
Symptoms of Heart Failure
Symptoms of heart failure can include:
- Shortness of breath noted during activity (most commonly) or at rest, especially when you lie down flat in bed.
- Cough that is productive of a white mucus.
- Quick weight gain (a weight gain of two or three pounds in one day is possible).
- Swelling in ankles, legs, and abdomen.
- Dizziness.
- Fatigue and weakness.
- Rapid or irregular heartbeats.
- Other symptoms include nausea, palpitations, and chest pain.
Like valve disease, heart failure symptoms may not be related to how weak your heart is. You may have many symptoms, but your heart function may be only mildly weakened. Or you may have a severely damaged heart, with little or no symptoms.
Symptoms of Congenital Heart Defects
Congenital heart defects may be diagnosed before birth, right after birth, during childhood, or not until adulthood. It is possible to have a defect and no symptoms at all. Sometimes it can be diagnosed because of a heart murmur on physical exam or an abnormal EKG or chest X-ray in someone with no symptoms.
In adults, if symptoms of congenital heart disease are present, they may include:
- Shortness of breath.
- Limited ability to exercise.
- Symptoms of heart failure (see above) or valve disease (see above).
Congenital Heart Defects in Infants and Children
Symptoms of congenital heart defects in infants and children may include:
- Cyanosis (a bluish tint to the skin, fingernails, and lips).
- Fast breathing and poor feeding.
- Poor weight gain.
- Recurrent lung infections.
- Inability to exercise.
Symptoms of Heart Muscle Disease (Cardiomyopathy)
Many people with cardiomyopathy have no symptoms or only minor symptoms, and live a normal life. Other people develop symptoms, which progress and worsen as heart function worsens.
Symptoms of cardiomyopathy can occur at any age and may include:
- Chest pain or pressure (occurs usually with exercise or physical activity, but can also occur with rest or after meals).
- Heart failure symptoms (see above).
- Swelling of the lower extremities.
- Fatigue.
- Fainting.
- Palpitations (fluttering in the chest due to abnormal heart rhythms).
Some people also have arrhythmias. These can lead to sudden death in a small number of people with cardiomyopathy.
Symptoms of Pericarditis
When present, symptoms of pericarditis may include:
- Chest pain. This pain is different from angina (pain caused by coronary artery disease). It may be sharp and located in the center of the chest. The pain may radiate to the neck and occasionally, the arms and back. It is made worse when lying down, taking a deep breath in, coughing, or swallowing and relieved by sitting forward.
-
Low-grade fever.
- Increased heart rate.
Because many of the symptoms associated with each type of heart disease are similar, it is important to see your doctor so that you can receive a correct diagnosis and prompt treatment.
Types of heart disease
Postado por Unknown | 04:31 | Angina pectoris, Cardiomyopathy, Cardiovascular Disorders, Conditions and Diseases, Coronary disease, Health, Heart disease, Myocardial infarction | 0 comentários » Image via Wikipedia
Image via Wikipedia
Coronary heart disease
Coronary artery disease is a disease of the artery caused by the accumulation of atheromatous plaques within the walls of the arteries that supply the myocardium. Angina pectoris (chest pain) and myocardial infarction (heart attack) are symptoms of and conditions caused by coronary heart disease.
Over 459,000 Americans die of coronary heart disease every year[5]. In the United Kingdom, 101,000 deaths annually are due to coronary heart disease.[6]
Cardiomyopathy
Cardiomyopathy literally means "heart muscle disease" (Myo= muscle, pathy= disease) It is the deterioration of the function of the myocardium (i.e., the actual heart muscle) for any reason. People with cardiomyopathy are often at risk of arrhythmia and/or sudden cardiac death.
- Extrinsic cardiomyopathies – cardiomyopathies where the primary pathology is outside the myocardium itself. Most cardiomyopathies are extrinsic, because by far the most common cause of a cardiomyopathy is ischemia. The World Health Organization calls these specific cardiomyopathies[citation needed]:
- Alcoholic cardiomyopathy
- Coronary artery disease
- Congenital heart disease – see below
- Nutritional diseases affecting the heart
- Ischemic (or ischaemic) cardiomyopathy
- Hypertensive cardiomyopathy
- Valvular cardiomyopathy – see also Valvular heart disease below
- Inflammatory cardiomyopathy – see also Inflammatory heart disease below
- Cardiomyopathy secondary to a systemic metabolic disease
- Intrinsic cardiomyopathies – weakness in the muscle of the heart that is not due to an identifiable external cause.
- Dilated cardiomyopathy (DCM) – most common form, and one of the leading indications for heart transplantation. In DCM the heart (especially the left ventricle) is enlarged and the pumping function is diminished.
- Hypertrophic cardiomyopathy (HCM or HOCM) – genetic disorder caused by various mutations in genes encoding sarcomeric proteins. In HCM the heart muscle is thickened, which can obstruct blood flow and prevent the heart from functioning properly.
- Arrhythmogenic right ventricular cardiomyopathy (ARVC) – arises from an electrical disturbance of the heart in which heart muscle is replaced by fibrous scar tissue. The right ventricle is generally most affected.
- Restrictive cardiomyopathy (RCM) – least common cardiomyopathy. The walls of the ventricles are stiff, but may not be thickened, and resist the normal filling of the heart with blood. ** Noncompaction Cardiomyopathy – the left ventricle wall has failed to properly grow from birth and such has a spongy appearance when viewed during an echocardiogram.
Cardiovascular disease
Cardiovascular disease is any of a number of specific diseases that affect the heart itself and/or the blood vessel system, especially the veins and arteries leading to and from the heart. Research on disease dimorphism suggests that women who suffer with cardiovascular disease usually suffer from forms that affect the blood vessels while men usually suffer from forms that affect the heart muscle itself. Known or associated causes of cardiovascular disease include diabetes mellitus, hypertension, hyperhomocysteinemia and hypercholesterolemia.
Types of cardiovascular disease include:
Ischaemic heart disease
- Ischaemic heart disease – another disease of the heart itself, characterized by reduced blood supply to the organs.
Heart failure
Heart failure, also called congestive heart failure (or CHF), and congestive cardiac failure (CCF), is a condition that can result from any structural or functional cardiac disorder that impairs the ability of the heart to fill with or pump a sufficient amount of blood throughout the body. Therefore leading to the heart and body's failure.
- Cor pulmonale, a failure of the right side of the heart.
Hypertensive heart disease
Hypertensive heart disease is heart disease caused by high blood pressure, especially localised high blood pressure. Conditions that can be caused by hypertensive heart disease include:
- Left ventricular hypertrophy
- Coronary heart disease
- (Congestive) heart failure
- Hypertensive cardiomyopathy
- Cardiac arrhythmias
Inflammatory heart disease
Inflammatory heart disease involves inflammation of the heart muscle and/or the tissue surrounding it.
- Endocarditis – inflammation of the inner layer of the heart, the endocardium. The most common structures involved are the heart valves.
- Inflammatory cardiomegaly
- Myocarditis – inflammation of the myocardium, the muscular part of the heart.
Valvular heart disease
Valvular heart disease is disease process that affects one or more valves of the heart. The valves in the right side of the heart are the tricuspid valve and the pulmonic valve. The valves in the left side of the heart are the mitral valve and the aortic valve.
See also
List of Heart Diseases
Postado por Unknown | 04:30 | Aortic valve, Atrial septal defect, Cardiomyopathy, Cardiovascular Disorders, Circulatory system, Conditions and Diseases, Health, Heart disease | 0 comentários »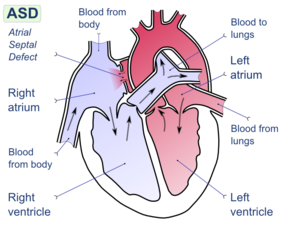 Image via Wikipedia
Image via Wikipedia
Aortic Dissection
Aortic dissection is a condition that is accompanied by severe chest pain. It requires immediate medical attention and usually requires surgery. In the initial stages of aortic dissection, the inner layer of the aorta develops a tear which allows blood to escape and pool at the outer aortic wall. If not treated quickly, the outer wall can rupture, resulting in rapid blood loss. Lack of immediate medical intervention can also cause the tear to spread and block a coronary artery, which leads to myocardial infarction.
Older people are at greater risk for aortic dissection, particularly if they have a history of hypertension, but younger people can develop this condition as well if they have specific inherited defects. One such inherited defect is Marfan's syndrome, which causes a weakening of the aortic wall that can lead to aortic dissection.
Cardiac Arrhythmia
Irregular beating of the heart, also called "arrhythmia," can show up in various ways. Patients may suffer from brief loss of consciousness ("syncope"), experience sensations of irregular or rapid heartbeats ("heart palpitations"), or feel light headed. A careful monitoring of the pulse or a routine ECG exam can detect many such forms of arrhythmias.
In another form of arrhythmia—atrioventricular block—the atrial contraction is not always followed by a ventricular contraction. This causes a slow heartbeat. "Atrioventricular block" can be caused by injury to the pacemaker fibers caused by myocardial infarction or viral diseases.
An abnormally long interval between the Q and the T wave (see the section on ECG) called "long QT syndrome," is another common type of arrhythmia and can occur from a variety of both inherited and non-inherited problems.
An abnormally short interval between heartbeats can be caused by premature contraction of the atrium due to an irregular spread of electrical activity of the ventricle.
Congenital Heart Diseases
When congenital heart disease shows up in the form of a malformed heart at birth, surgical repair is often possible to correct immediate problems.
Sometimes, however, congenital heart disease is not detected until adulthood. The most common such problem is an atrial septal defect ("ASD"). In ASD, the septum between the right and left atria has an opening. Typically, because the left heart circulation has higher pressure, blood is shunted from the left to the right atrium, resulting in increased pulmonary circulation and enlargement of the right heart. Symptoms of ASD may include breathlessness and arrhythmia. ASD can be diagnosed by echocardiography and X-ray, and sometimes by ECG.
Other more serious congenital heart diseases include various conditions that lead to cyanosis, in which a substantial mixing of oxygenated and deoxygenated blood occurs. An example of this is "tetralogy of Fallot," which is characterized by an obstruction of the pulmonary outflow combined with a ventricular septal defect, which together allow the mixing of blood between the left and right ventricles.
Myocardial Infarction (MI)
Myocardial infarction (MI), commonly known as a "heart attack," occurs when a patch of heart muscle dies because of a sudden blockage of a coronary artery (coronary thrombosis). It is usually accompanied by crushing chest pain, and often by some evidence of heart malfunction.
Blocking of the coronary arteries is most often due to a condition called "atherosclerosis," which is a buildup of fatty substances in the bloodstream along the inner layer of the arteries over time that restricts blood flow to the heart. These substances can also create an abnormal mass of platelets which become blood clots.
The resulting scar tissue from the dead muscle with MI alters the pattern of electrical activity of the heart. These changes in electrical patterns show up clearly in an electrocardiogram (ECG) exam, making it the most important tool available for diagnosing MI.
Cardiomyopathies
Dilated Cardiomyopathy
This is the most common of the diseases of the heart muscle. In dilated cardiomyopathy, the contraction of the heart muscle is weakened and the left ventricle becomes dilated as a result, leading to reduced blood output.
Dilated cardiomyopathy may develop from many different causes. For example, weakening of the heart muscle can be caused by coronary artery obstruction, which leads to loss of muscle tissue and scarring. Alternatively, infections by agents such as Lyme disease can inflame the heart muscles and cause them to lose strength. Chemicals such as alcohol or cocaine can also lead to this condition.
Dilated cardiomyopathy can be detected most effectively by using an echocardiogram exam to measure ventricular volume, thickness, and function. However, X-ray or ECG exams can also help with detection.
Hypertrophic Cardiomyopathy
In this disease the muscle tissue in the septum that separates the two ventricles become abnormally thickened. The end result is that the ventricular volume is drastically reduced and a smaller amount of blood is ejected from the ventricle at a much higher speed. The speed of ejection and the narrowness of the path of ejection inside the ventricle cause a murmur that can be heard during systole. In addition, the reduced volume of the chamber can interfere with the normal workings of the mitral valve, and mitral regurgitation can occur.
Hypertrophic cardiomyopathy can be caused by hypertension or aortic stenosis, particularly in older people. It may also occur in younger people as a genetically inherited trait known as "familial hypertrophic cardiomyopathy." This disease can often be detected as a heart murmur, but the best diagnostic test is echocardiography, which allows for the measurements of abnormal anatomy and blood flow. The first symptoms of this disease are angina, syncope, ventricular failure, or sudden death.
Valvular Diseases
Aortic Regurgitation
In aortic regurgitation, the aortic valves do not close properly and they allow blood to flow back into the left ventricle. This condition can be caused by diseases of the aortic valves themselves, such as rheumatic heart disease, or by problems with the support structures above the valve, such as aortic aneurysm. The result is a reduction in pumping efficiency, which can lead to dilation of the left ventricle and breathlessness.
Regurgitation can be detected as a blowing murmur (sort of a harsh, whooshing sound), and the timing of the murmur can determine whether it is associated with mitral or aortic valves (unless the valve problems are in the right heart). Echocardiography, particularly the Doppler version showing blood flow, is a very effective technique for diagnosing this condition.
Aortic Stenosis
This obstruction of the outflow from the left ventricle can occur as a defect of the aortic valve itself, or be caused by an obstruction above or below the valve. Obstructed outflow increases the left ventricular pressure and also leads to hypertrophic cardiomyopathy. When valvular aortic stenosis occurs in childhood it is most often congenital, as is most aortic stenosis that occurs above and below the aortic valve. When aortic stenosis occurs in old age it is usually caused by hardening of the valves.
This condition can be detected as murmurs when there is an obstruction of the left ventricular outflow. Usual symptoms for patients suffering from aortic stenosis are angina, breathlessness, and brief loss of consciousness (syncope).
Mitral Regurgitation
Much like aortic regurgitation, mitral regurgitation can be caused by diseases directly affecting the mitral valves. It can also be caused indirectly by other conditions such as hypertrophic cardiomyopathy.
Floppy valve, also known as "mitral valve prolapse," can be caused by diseases of the connective tissue such as Marfan syndrome. In such cases, the floppy valve can produce clicking sounds during systole as the valves balloon into the atrium. The actual regurgitation sounds are blowing murmurs during systole (the pumping phase).
Other causes of mitral regurgitation include damage to the muscles attached to the mitral valves, rheumatic disease, and calcification of the opening between the left atrium and left ventricle. Apart from the characteristic sounds, mitral regurgitation can be easily detected by Doppler echocardiography.
Mitral Stenosis
The main cause of mitral stenosis in adults is rheumatic heart disease. In these cases, an acute childhood rheumatic fever causes the mitral valves to become calcified and to thicken, which leads to a progressively narrower opening into the left ventricle.
Rheumatic fever is now rare in developed countries, so most occurrences of this disease are in elderly people who suffered rheumatic fever when young. In developing countries, rheumatic fever is still a problem, and the resulting mitral stenosis can cause problems in young people during conditions of circulatory stress such as pregnancy or extreme physical exertion.
Mitral stenosis can be detected by listening to the heart: the first sound is accentuated, while the second sound is followed by an opening snap of the valves. In addition, a rumbling sound may be heard during diastole (which is when the heart relaxes between beats). Echocardiography may reveal thickened mitral valves.
Inherited Heart Diseases
Many of the diseases or conditions described so far can occur as a result of a genetically inherited trait. This section lists some of these heritable diseases. Many of these diseases are not specific to the heart, but stem from a more generalized problem which happens to affect the heart.Ellis-van Creveld Syndrome
This syndrome represents a rare autosomal recessive trait. The fact that it is found more commonly among the Amish people is explained by the founder effect, which occurs when a gene pool is restricted because the population is relatively isolated and has descended from a few individuals.
Ellis-van Creveld syndrome is characterized by atrial septal defects (see congenital heart defects) which in severe cases result in the affected individual having a single combined atrium. Other manifestations of this disease include extra digits and dwarfism.
Familial Hypertrophic Cardiomyopathy
Discussed in the previous cardiomyopathies section. More than 40 mutations have been identified that cause the familial form of hypertrophic cardiomyopathy. These are inherited as autosomal (non sex-linked) dominant traits.
Holt-Orams Syndrome
While this autosomal dominant disorder can cause arm abnormalities, it also manifests as an atrial septal defect (ASD) of varying severity. The electrical activity of the heart may also be disturbed due to the ASD.
Marfan Syndrome
This is an autosomal dominant disorder of varying severity. The disease affects the connective tissue and results in the abnormal length of the extremities: legs, arms, fingers, and toes. Affected individuals may also have problems with their eyes. Marfan syndrome can cause aortic aneurysm and aortic dissection as well as mitral regurgitation and aortic regurgitation.
Ward-Romano Syndrome
This is a form of long QT syndrome (see cardiac arrhythmia and ECG ) that is inherited as an autosomal dominant trait. At least three different genes have been identified, mutations in which can lead to this disease.
The long QT interval results from abnormal electrical conduction in the heart and can lead to brief loss of consciousness (syncope) and sudden death.
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_e.png?x-id=d2f78067-4f9a-43b6-bb0f-915b3cd1ead1)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_e.png?x-id=8394c95a-062e-4de8-8fcd-22605f3a45e8)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_e.png?x-id=695346d5-91d3-4d5c-b3e8-92c3ae0ea94b)
![Reblog this post [with Zemanta]](http://img.zemanta.com/reblog_e.png?x-id=a4f8a7b8-5acb-4656-a3f9-a0bccf64bd2f)


